Understand Heel Painfulness
Overview

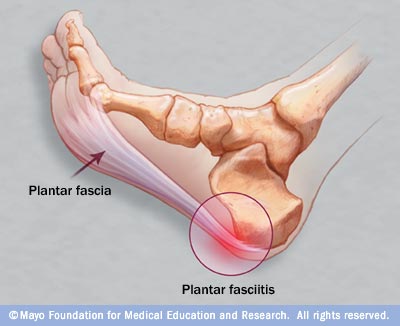
Pain arises in the centre of the heel and sometimes can spread to the arch region of the foot. Some patients complain of intense Heel Pain when walking the first few steps in the morning and after periods of rest. The most common cause of heel pain is plantar fascitis. The plantar fascia is a broad band of tissue that runs along the bottom of the foot. When this band of tissue is damaged due to biomechanical reasons or inappropriate running shoes then the tissue can become inflamed or even tear at the heel bone. This can be very painful.
Causes
Some of the many causes of heel pain can include abnormal walking style (gait), such as rolling the feet inwards. Obesity. Ill-fitting shoes. Standing, running or jumping on hard surfaces. Injury to the heel, such as stress fractures. Bursitis (inflammation of a bursa, bursae are small sacs that contain fluid to lubricate moving parts, such as joints and muscles). Neuroma (nerve enlargement). Certain disorders, including diabetes and arthritis.
Symptoms
Plantar fascia usually causes pain and stiffness on the bottom of your heel although some people have heel spurs and suffer no symptoms at all. Occasionally, heel pain is also associated with other medical disorders such as arthritis (inflammation of the joint), bursitis (inflammation of the tissues around the joint). Those who have symptoms may experience ?First step? pain (stone bruise sensation) after getting out of bed or sitting for a period of time. Pain after driving. Pain on the bottom of your heel. Deep aching pain. Pain can be worse when barefoot.
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Essentially rest from aggravating activity, physiotherapy treatment to alleviate the inflammatory component, stretching the tight calf, strengthening up of the intrinsic muscles of the foot e.g. tissue scrunch, picking up pens etc. and correction of biomechanical problems in the foot e.g. orthotics. Sometimes, a heel cup or pad to relieve pressure - a donut type pad may be helpful. Strapping has been shown to be helpful, especially in circumstances where the patient can?t wear orthotics - the foot is strapped to help support the arch. There has been limited success with cortisone injections or surgery and the latter is very rarely required.
Surgical Treatment
Surgery to correct heel pain is generally only recommended if orthotic treatment has failed. There are some exceptions to this course of treatment and it is up to you and your doctor to determine the most appropriate course of treatment. Following surgical treatment to correct heel pain the patient will generally have to continue the use of orthotics. The surgery does not correct the cause of the heel pain. The surgery will eliminate the pain but the process that caused the pain will continue without the use of orthotics. If orthotics have been prescribed prior to surgery they generally do not have to be remade.
Prevention

Wear properly fitting shoes. Place insoles or inserts in your shoes to help control abnormal foot motion. Maintain a healthy weight. Exercise and do foot stretches as they have been shown to decrease the incidence of heel pain.

Pain arises in the centre of the heel and sometimes can spread to the arch region of the foot. Some patients complain of intense Heel Pain when walking the first few steps in the morning and after periods of rest. The most common cause of heel pain is plantar fascitis. The plantar fascia is a broad band of tissue that runs along the bottom of the foot. When this band of tissue is damaged due to biomechanical reasons or inappropriate running shoes then the tissue can become inflamed or even tear at the heel bone. This can be very painful.
Causes
Some of the many causes of heel pain can include abnormal walking style (gait), such as rolling the feet inwards. Obesity. Ill-fitting shoes. Standing, running or jumping on hard surfaces. Injury to the heel, such as stress fractures. Bursitis (inflammation of a bursa, bursae are small sacs that contain fluid to lubricate moving parts, such as joints and muscles). Neuroma (nerve enlargement). Certain disorders, including diabetes and arthritis.
Symptoms
Plantar fascia usually causes pain and stiffness on the bottom of your heel although some people have heel spurs and suffer no symptoms at all. Occasionally, heel pain is also associated with other medical disorders such as arthritis (inflammation of the joint), bursitis (inflammation of the tissues around the joint). Those who have symptoms may experience ?First step? pain (stone bruise sensation) after getting out of bed or sitting for a period of time. Pain after driving. Pain on the bottom of your heel. Deep aching pain. Pain can be worse when barefoot.
Diagnosis
Your doctor will perform a physical exam and ask questions about your medical history and symptoms, such as have you had this type of heel pain before? When did your pain begin? Do you have pain upon your first steps in the morning or after your first steps after rest? Is the pain dull and aching or sharp and stabbing? Is it worse after exercise? Is it worse when standing? Did you fall or twist your ankle recently? Are you a runner? If so, how far and how often do you run? Do you walk or stand for long periods of time? What kind of shoes do you wear? Do you have any other symptoms? Your doctor may order a foot x-ray. You may need to see a physical therapist to learn exercises to stretch and strengthen your foot. Your doctor may recommend a night splint to help stretch your foot. Surgery may be recommended in some cases.
Non Surgical Treatment
Essentially rest from aggravating activity, physiotherapy treatment to alleviate the inflammatory component, stretching the tight calf, strengthening up of the intrinsic muscles of the foot e.g. tissue scrunch, picking up pens etc. and correction of biomechanical problems in the foot e.g. orthotics. Sometimes, a heel cup or pad to relieve pressure - a donut type pad may be helpful. Strapping has been shown to be helpful, especially in circumstances where the patient can?t wear orthotics - the foot is strapped to help support the arch. There has been limited success with cortisone injections or surgery and the latter is very rarely required.
Surgical Treatment
Surgery to correct heel pain is generally only recommended if orthotic treatment has failed. There are some exceptions to this course of treatment and it is up to you and your doctor to determine the most appropriate course of treatment. Following surgical treatment to correct heel pain the patient will generally have to continue the use of orthotics. The surgery does not correct the cause of the heel pain. The surgery will eliminate the pain but the process that caused the pain will continue without the use of orthotics. If orthotics have been prescribed prior to surgery they generally do not have to be remade.
Prevention

Wear properly fitting shoes. Place insoles or inserts in your shoes to help control abnormal foot motion. Maintain a healthy weight. Exercise and do foot stretches as they have been shown to decrease the incidence of heel pain.
What's The Primary Cause Of Achilles Tendonitis Pain ?
Overview
 Achilles Tendonitis is an inflammation of the Achilles tendon, which attaches the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). Pain can be felt on the back of the heel at the attachment of the tendon, along the length of the tendon, or at the base of the calf where the tendon attaches to the muscle. Swelling is not always present with this injury, but it may occur in severe cases.
Achilles Tendonitis is an inflammation of the Achilles tendon, which attaches the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). Pain can be felt on the back of the heel at the attachment of the tendon, along the length of the tendon, or at the base of the calf where the tendon attaches to the muscle. Swelling is not always present with this injury, but it may occur in severe cases.
Causes
In some cases, Achilles Tendinitis can be caused by physical activity without a proper warm up or trauma, such as falling, to cause an overstressing of the muscle and tendon. Other causes include repetitive overuse syndrome, such as a job that required frequent heel lifting. Biomechanical causes such as pronation (or fallen arches) will cause the heel (calcaneus) to lean slightly, putting the undue stress on the Achilles tendon and the calf muscles. Most pain can be felt at the back of the heel or the point at which the calf muscle becomes a tendon three quarters of the distance down from the knee. Discomfort can be felt especially when jumping or when lifting the heel off the ground. Swelling and redness can often be seen at the back of the heel and touching the area would cause a tender sensation. In extreme cases, the tendon can become torn or rupture entirely which would cause bruising or an inability to put pressure on the foot.
Symptoms
Common symptoms of Achilles tendinitis include weakness in the leg, slight pain above the heel in the lower leg after activity, feeling of stiffness in the leg that usually appears in the morning and lessens throughout the day, bad pain the day after exercising, pain as you climb stairs or go uphill, swelling in the area of the Achilles tendon, creaking or cracking noise when you press on the Achilles tendon.
Diagnosis
Your physiotherapist or sports doctor can usually confirm the diagnosis of Achilles tendonitis in the clinic. They will base their diagnosis on your history, symptom behaviour and clinical tests. Achilles tendons will often have a painful and prominent lump within the tendon. Further investigations include US scan or MRI. X-rays are of little use in the diagnosis.
Nonsurgical Treatment
In order to treat achilles tendinitis effectively, it is important to complete a thorough examination of the entire lower extremity. Once the true cause is identified, a comprehensive treatment program can be initiated to reduce inflammation and improve any faulty lower extremity biomechanics. Treatment options may include biomechanical analysis of gait. Splinting/bracing to alleviate the strain on the tendon. Soft tissue mobilization/manual therapy to decrease inflammation and promote healing of the tendon. Strengthening/flexibility and proprioceptive exercises. Home exercise program. Modalities for pain and inflammation (i.e. ultrasound, iontophoresis, electrical stimulation, ice). Methods to alter faulty mechanics (i.e taping, orthotics). Education about lifestyle changes (i.e. proper shoes, activity modification).

Surgical Treatment
Surgery can be done to remove hardened fibrous tissue and repair any small tendon tears as a result of repetitive use injuries. This approach can also be used to help prevent an Achilles tendon rupture. If your Achilles tendon has already ruptured or torn, Achilles tendon surgery can be used to reattach the ends of the torn tendon. This approach is more thorough and definitive compared to non surgical treatment options discussed above. Surgical reattachment of the tendon also minimizes the change of re-rupturing the Achilles tendon.
Prevention
To prevent Achilles tendonitis or tendonosis from recurring after surgical or non-surgical treatment, the foot and ankle surgeon may recommend strengthening and stretching of the calf muscles through daily exercises. Wearing proper shoes for the foot type and activity is also important in preventing recurrence of the condition.
 Achilles Tendonitis is an inflammation of the Achilles tendon, which attaches the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). Pain can be felt on the back of the heel at the attachment of the tendon, along the length of the tendon, or at the base of the calf where the tendon attaches to the muscle. Swelling is not always present with this injury, but it may occur in severe cases.
Achilles Tendonitis is an inflammation of the Achilles tendon, which attaches the calf muscles (gastrocnemius and soleus) to the heel bone (calcaneus). Pain can be felt on the back of the heel at the attachment of the tendon, along the length of the tendon, or at the base of the calf where the tendon attaches to the muscle. Swelling is not always present with this injury, but it may occur in severe cases.
Causes
In some cases, Achilles Tendinitis can be caused by physical activity without a proper warm up or trauma, such as falling, to cause an overstressing of the muscle and tendon. Other causes include repetitive overuse syndrome, such as a job that required frequent heel lifting. Biomechanical causes such as pronation (or fallen arches) will cause the heel (calcaneus) to lean slightly, putting the undue stress on the Achilles tendon and the calf muscles. Most pain can be felt at the back of the heel or the point at which the calf muscle becomes a tendon three quarters of the distance down from the knee. Discomfort can be felt especially when jumping or when lifting the heel off the ground. Swelling and redness can often be seen at the back of the heel and touching the area would cause a tender sensation. In extreme cases, the tendon can become torn or rupture entirely which would cause bruising or an inability to put pressure on the foot.
Symptoms
Common symptoms of Achilles tendinitis include weakness in the leg, slight pain above the heel in the lower leg after activity, feeling of stiffness in the leg that usually appears in the morning and lessens throughout the day, bad pain the day after exercising, pain as you climb stairs or go uphill, swelling in the area of the Achilles tendon, creaking or cracking noise when you press on the Achilles tendon.
Diagnosis
Your physiotherapist or sports doctor can usually confirm the diagnosis of Achilles tendonitis in the clinic. They will base their diagnosis on your history, symptom behaviour and clinical tests. Achilles tendons will often have a painful and prominent lump within the tendon. Further investigations include US scan or MRI. X-rays are of little use in the diagnosis.
Nonsurgical Treatment
In order to treat achilles tendinitis effectively, it is important to complete a thorough examination of the entire lower extremity. Once the true cause is identified, a comprehensive treatment program can be initiated to reduce inflammation and improve any faulty lower extremity biomechanics. Treatment options may include biomechanical analysis of gait. Splinting/bracing to alleviate the strain on the tendon. Soft tissue mobilization/manual therapy to decrease inflammation and promote healing of the tendon. Strengthening/flexibility and proprioceptive exercises. Home exercise program. Modalities for pain and inflammation (i.e. ultrasound, iontophoresis, electrical stimulation, ice). Methods to alter faulty mechanics (i.e taping, orthotics). Education about lifestyle changes (i.e. proper shoes, activity modification).

Surgical Treatment
Surgery can be done to remove hardened fibrous tissue and repair any small tendon tears as a result of repetitive use injuries. This approach can also be used to help prevent an Achilles tendon rupture. If your Achilles tendon has already ruptured or torn, Achilles tendon surgery can be used to reattach the ends of the torn tendon. This approach is more thorough and definitive compared to non surgical treatment options discussed above. Surgical reattachment of the tendon also minimizes the change of re-rupturing the Achilles tendon.
Prevention
To prevent Achilles tendonitis or tendonosis from recurring after surgical or non-surgical treatment, the foot and ankle surgeon may recommend strengthening and stretching of the calf muscles through daily exercises. Wearing proper shoes for the foot type and activity is also important in preventing recurrence of the condition.
What Causes Painful Heel And How To Overcome It

Overview
The Plantar Fascia is a broad, thick band of tissue that runs from under the heel to the front of the foot. Through overuse the fascia can become inflamed and painful at its attachment to the heel bone or calcaneus. The condition is traditionally thought to be inflammation, however this is now believed to be incorrect due to the absence of inflammatory cells within the fascia. The cause of pain is thought to be degeneration of the collagen fibres close to the attachment to the heel bone.
Causes
Plantar fasciitis tends to strike those who overtrain, neglect to stretch their calf muscles, or overdo hill work and speedwork. Plantar fasciitis can also be caused by biomechanical flaws, including flat, high-arched feet and a tight Achilles tendon; excessive pronation; sudden increases in training mileage; beginning speedwork; wearing worn running shoes; running on hard surfaces, like asphalt or concrete; or wearing high heels all day before switching into flat running shoes.
Symptoms
If you have Plantar Fasciitis, you will most likely feel a sharp pain under the ball of you heel and it will often give pain when standing after a period of rest. For example when you get out of bed in the mornings or after being sat down. Some patients describe this feeling as a stone bruise sensation, or a pebble in the shoe and at times the pain can be excruciating. Patients with Plantar Fasciitis can experience pain free periods whereby the think they are on the mend, only for the heel pain to come back aggressively when they appear to have done nothing wrong. If your plantar fasciitis came on very suddenly and the pain is relentless, then you may have Plantar Fascial Tears. We will be able to differentiate between these 2 conditions, sometimes with ultra sound imaging. The treatment for each of these conditions will need to be very different.
Diagnosis
A physical exam performed in the office along with the diagnostic studies as an x-ray. An MRI may also be required to rule out a stress fracture, or a tear of the plantar fascia. These are conditions that do not normally respond to common plantar fasciitis treatment.
Non Surgical Treatment
Check your shoes to make sure they offer sufficient support and motion control. They should bend only at the ball of the foot, where your toes attach to the foot. This is very important. Avoid any shoe that bends in the center of the arch or behind the ball of the foot. It offers insufficient support and will stress your plantar fascia. The human foot was not designed to bend here and neither should a shoe be designed to do this. You may also strengthen the muscles in your arch by performing toe curls or "doming". Toe curls may be done by placing a towel on a kitchen floor and then curling your toes to pull the towel towards you. This exercise may also be done without the towel against the resistance of the floor. Plantar fasciitis is usually controlled with conservative treatment. Besides surgery and cortisone injections, physical therapy modalities such as electrical stimulation and ultrasound can be used. Often the foot will be taped to limit pronation. Following control of the pain and inflammation an orthotic (a custom made shoe insert) can be used to control over-pronation.

Surgical Treatment
In very rare cases plantar fascia surgery is suggested, as a last resort. In this case the surgeon makes an incision into the ligament, partially cutting the plantar fascia to release it. If a heel spur is present, the surgeon will remove it. Plantar Fasciitis surgery should always be considered the last resort when all the conventional treatment methods have failed to succeed. Endoscopic plantar fasciotomy (EPF) is a form of surgery whereby two incisions are made around the heel and the ligament is being detached from the heel bone allowing the new ligament to develop in the same place. In some cases the surgeon may decide to remove the heel spur itself, if present. Just like any type of surgery, Plantar Fascia surgery comes with certain risks and side effects. For example, the arch of the foot may drop and become weak. Wearing an arch support after surgery is therefore recommended. Heel spur surgeries may also do some damage to veins and arteries of your foot that allow blood supply in the area. This will increase the time of recovery.
Prevention
Factors that help prevent plantar fasciitis and reduce the risk of recurrence include. Exercises to strengthen the muscles of the lower leg and ankle. Warming up before commencing physical activity. Maintaining a healthy body weight. Avoiding high heeled footwear. Using orthotic devices such as arch supports and heel raises in footwear, particularly for people with very high arches or flat feet. Daily stretches of plantar fascia and Achilles tendon.
What Can Cause Plantar Fasciitis To Appear

Overview
The plantar fascia is a band of connective tissue on the bottom of the foot that helps form the arch of the foot. Acute injury or cumulative trauma to the plantar fascia can be a cause of inflammation and heel pain. This is called plantar fasciitis.
Causes
Your plantar fascia (fay-sha) supports the arch of your foot as you run or walk. It is a thick, inelastic, fibrous band that starts in your heel, runs along the bottom of your foot, and spreads out to your toes. Plantar fasciitis is an inflammation of this fibrous band. If you are female or have a job that requires a lot of walking or standing on hard surfaces you are more at risk for plantar fasciitis. Additional causes include Being overweight, Having flat feet or high arches, Wearing shoes with poor support, Walking or running for exercise, Tight calf muscles that limit how far you can flex your ankles, Running on soft terrain, Increase in activity level, Genetic predisposition.
Symptoms
Pain tends to start gradually, often just in the heel, but it can sometimes be felt along the whole of the plantar fascia. The symptoms are initially worse in the morning and mostly after, rather than during, activity. As the condition becomes worse, the symptoms become more persistent.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process the surgeon rules out all the possible causes for your heel pain other than plantar fasciitis. In addition, diagnostic imaging studies such as x-rays or other imaging modalities may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
Non Surgical Treatment
Treatment of plantar fasciitis is sometimes a drawn out and frustrating process. A program of rehabilitation should be undertaken with the help of someone qualified and knowledgeable about the affliction. Typically, plantar fasciitis will require at least six weeks and up to six months of conservative care to be fully remedied. Should such efforts not provide relief to the athlete, more aggressive measures including surgery may be considered. The initial goals of physical therapy should be to increase the passive flexion of the foot and improve flexibility in the foot and ankle, eventually leading to a full return to normal function. Prolonged inactivity in vigorous sports is often the price to be paid for thorough recovery. Half measures can lead to a chronic condition, in some cases severely limiting athletic ability. As a large amount of time is spent in bed during sleeping hours, it is important to ensure that the sheets at the foot of the bed do not constrict the foot, leading to plantar flexion in which the foot is bent straight out with the toes pointing. This constricts and thereby shortens the gastroc complex, worsening the condition. A heating pad placed under the muscles of the calf for a few minutes prior to rising may help loosen tension, increase circulation in the lower leg and reduce pain. Also during sleep, a night splint may be used in order to hold the ankle joint in a neutral position. This will aid in the healing of the plantar fascia and ensure that the foot will not become flexed during the night.
Surgical Treatment
Surgery is usually not needed for plantar fasciitis. About 95 out of 100 people who have plantar fasciitis are able to relieve heel pain without surgery. Your doctor may consider surgery if non-surgical treatment has not helped and heel pain is restricting your daily activities. Some doctors feel that you should try non-surgical treatment for at least 6 months before you consider surgery. The main types of surgery for plantar fasciitis are Plantar fascia release. This procedure involves cutting part of the plantar fascia ligament . This releases the tension on the ligament and relieves inflammation . Other procedures, such as removing a heel spur or stretching or loosening specific foot nerves. These surgeries are usually done in combination with plantar fascia release when there is lasting heel pain and another heel problem. Experts in the past thought that heel spurs caused plantar fasciitis. Now experts generally believe that heel spurs are the result, not the cause, of plantar fasciitis. Many people with large heel spurs never have heel pain or plantar fasciitis. So surgery to remove heel spurs is rarely done.
Prevention
Stretching the plantar fascia and the calf muscle area can help to prevent inflammation. Slowly increasing the amount or intensity of athletic activities by graded progression can also help to prevent injury. Recommended Stretches: Taking a lunge position with the injured foot behind and keeping your heels flat on the floor, lean into a wall and bend the knees. A stretch should be felt in the sole and in the Achilles tendon area. Hold the stretch for 20-30 seconds. Also try this stretch with the back leg straight.
What Is Pain Of The Heel And Methods To Fix It

Overview
Heel pain is most often caused by plantar fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation, or, rarely, a cyst. Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and determine the underlying source of your heel pain. Plantar fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
Causes
Plantar fasciitis occurs because of irritation to the thick ligamentous connective tissue that runs from the heel bone to the ball of the foot. This strong and tight tissue contributes to maintaining the arch of the foot. It is also one of the major transmitters of weight across the foot as you walk or run. Therefore, the stress placed on the this tissue is tremendous.
Symptoms
The major complaint of those with plantar fasciitis is pain and stiffness in the bottom of the heel. This develops gradually over time. It usually affects just one foot, but can affect both feet. Some people describe the pain as dull, while others experience a sharp pain, and some feel a burning or ache on the bottom of the foot extending outward from the heel. The pain is usually worse in the morning when you take your first steps out of bed, or if you’ve been sitting or lying down for a while. Climbing stairs can be very difficult due to the heel stiffness. After prolonged activity, the pain can flare-up due to increased inflammation. Pain is not usually felt during the activity, but rather just after stopping.
Diagnosis
Diagnosis of plantar fasciitis is based on a medical history, the nature of symptoms, and the presence of localised tenderness in the heel. X-rays may be recommended to rule out other causes for the symptoms, such as bone fracture and to check for evidence of heel spurs. Blood tests may also be recommended.
Non Surgical Treatment
Plantar fasciitis treatment can be conservative (non-surgical) or invasive (surgical). Among the non-surgical ways to manage plantar fasciitis involves stretching and icing exercises. A night splint which help stretch the Achilles tendon and plantar fascia overnight, so that they can be more easily stretched during the morning. Orthotics that can be custom-made for the feet can also distribute tension on the feet more consistently. Corticosteroid is injected into the affected area to relieve pain and decrease inflammation. Doctors may also use extracorporeal shockwave therapy before considering plantar fasciitis surgery. During the therapy, sound waves are used to stimulate the affected area and eventually heal it. Physical therapy incorporation, deep massage stretching, and other modalities can at times be a helpful adjunct treatment. Surgery for plantar fasciitis is only considered when all other conservative treatments have failed.

Surgical Treatment
Surgery is rarely used in the treatment of plantar fasciitis. However it may be recommended when conservative treatment has been tried for several months but does not bring adequate relief of symptoms. Surgery usually involves the partial release of the plantar fascia from the heel bone. In approximately 75% of cases symptoms are fully resolved within six months. In a small percentage of cases, symptoms may take up to 12 months to fully resolve.
What Causes Heel Pain To Appear
Overview
The plantar fascia is a strong, relatively inflexible, fibrous ligament band that runs through the bottom of the foot. That band helps to keep the complex arch system of the foot, absorb shock, plays a role in body balance and in the various phases of gait. The band transmits your weight across the bottom of the foot with each step you take. When the heel of the trailing leg starts to get off the ground, the band bears tension that is approximately twice the body weight. The tension on the band at this moment is even greater if the calf muscles are not flexible enough.
Causes
Plantar fasciitis is caused by drastic or sudden increases in mileage, poor foot structure, and inappropriate running shoes, which can overload the plantar fascia, the connective tissue that runs from the heel to the base of the toes. The plantar fascia may look like a series of fat rubber bands, but it's made of collagen, a rigid protein that's not very stretchy. The stress of overuse, overpronation, or overused shoes can rip tiny tears in it, causing pain and inflammation, a.k.a. plantar fasciitis.
Symptoms
People with this condition sometimes describe the feeling as a hot, sharp sensation in the heel. You usually notice the pain first thing in the morning when you stand. After walking for a period of time, the pain usually lessens or even disappears. However, sharp pain in the center of the heel may return after resting for a period of time and then resuming activity.
Diagnosis
A physical exam performed in the office along with the diagnostic studies as an x-ray. An MRI may also be required to rule out a stress fracture, or a tear of the plantar fascia. These are conditions that do not normally respond to common plantar fasciitis treatment.
Non Surgical Treatment
Treatment of plantar fasciitis begins with first-line strategies, which you can begin at home. Stretching exercises. Exercises that stretch out the calf muscles help ease pain and assist with recovery. Avoid going barefoot. When you walk without shoes, you put undue strain and stress on your plantar fascia. Ice. Putting an ice pack on your heel for 20 minutes several times a day helps reduce inflammation. Place a thin towel between the ice and your heel,do not apply ice directly to the skin. Limit activities. Cut down on extended physical activities to give your heel a rest. Shoe modifications. Wearing supportive shoes that have good arch support and a slightly raised heel reduces stress on the plantar fascia. Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation. If you still have pain after several weeks, see your foot and ankle surgeon, who may add one or more of these treatment approaches. Padding and strapping. Placing pads in the shoe softens the impact of walking. Strapping helps support the foot and reduce strain on the fascia. Orthotic devices. Custom orthotic devices that fit into your shoe help correct the underlying structural abnormalities causing the plantar fasciitis. Injection therapy. In some cases, corticosteroid injections are used to help reduce the inflammation and relieve pain. Removable walking cast. A removable walking cast may be used to keep your foot immobile for a few weeks to allow it to rest and heal. Night splint. Wearing a night splint allows you to maintain an extended stretch of the plantar fascia while sleeping. This may help reduce the morning pain experienced by some patients. Physical therapy. Exercises and other physical therapy measures may be used to help provide relief.

Surgical Treatment
The most dramatic therapy, used only in cases where pain is very severe, is surgery. The plantar fascia can be partially detached from the heel bone, but the arch of the foot is weakened and full function may be lost. Another surgery involves lengthening the calf muscle, a process called gastrocnemius recession. If you ignore the condition, you can develop chronic heel pain. This can change the way you walk and cause injury to your legs, knees, hips and back. Steroid injections and some other treatments can weaken the plantar fascia ligament and cause potential rupture of the ligament. Surgery carries the risks of bleeding, infection, and reactions to anesthesia. Plantar fascia detachment can also cause changes in your foot and nerve damage. Gastrocnemius resection can also cause nerve damage.
Stretching Exercises
The following exercises are commonly prescribed to patients with this condition. You should discuss the suitability of these exercises with your physiotherapist prior to beginning them. Generally, they should be performed 2 - 3 times daily and only provided they do not cause or increase symptoms. Your physiotherapist can advise when it is appropriate to begin the initial exercises and eventually progress to the intermediate and advanced exercises. As a general rule, addition of exercises or progression to more advanced exercises should take place provided there is no increase in symptoms. Calf Stretch with Towel. Begin this stretch in long sitting with your leg to be stretched in front of you. Your knee and back should be straight and a towel or rigid band placed around your foot as demonstrated. Using your foot, ankle and the towel, bring your toes towards your head until you feel a stretch in the back of your calf, Achilles tendon, plantar fascia or leg. Hold for 5 seconds and repeat 10 times at a mild to moderate stretch provided the exercise is pain free. Resistance Band Calf Strengthening. Begin this exercise with a resistance band around your foot as demonstrated and your foot and ankle held up towards your head. Slowly move your foot and ankle down against the resistance band as far as possible and comfortable without pain, tightening your calf muscle. Very slowly return back to the starting position. Repeat 10 - 20 times provided the exercise is pain free.
Symptoms Of Pes Cavus
Pain across the bottom of the foot at any point between the heel and the ball of the foot is often referred to as "arch pain” Although this description is non-specific, most arch pain is due to strain or inflammation Foot Hard Skin of the plantar fascia (a long ligament on the bottom of the foot). Wearing inappropriate footwear or foot problems like athlete's foot and Morton's neuroma are some of the factors that cause burning feet sensation.
These conditions include different types of arthritis , osteonecrosis , neuromas , tumors, or infections. Lastly, traumatic injuries, including fractures and ligament tears, can cause this type of foot pain. Treatment of foot pain often consists of anti-inflammatory medications , footwear modifications, and inserts for your shoes. When buying footwear, look for shoes with a wide toebox, good support, and avoid high heels. These pads help to take pressure off the ball of the foot. If some simple steps do not alleviate your symptoms, you should see your doctor to ensure you are receiving adequate treatment. In some rare situations, patients don't find relief with shoe modifications, and may require a surgical procedure. Remember that our shoes protect us from injury.
When the tissue of the arch of the foot becomes irritated and inflamed, even simple movements can be quite painful. Plantar fasciitis is the name that describes inflammation of the fibrous band of tissue that connects the heel to the toes. Symptoms of plantar fasciitis include pain early in the morning and pain with long walks or prolonged standing. Arch pain early in the morning is due to the plantar fascia becoming contracted and tight as you sleep through the night. Bunions develop from a weakness in the bone structure of your foot.
Rheumatoid arthritis causes forefoot deformity and often may cause displacement and even dislocation of the metatarsal joints themselves. Morton's Neuroma can also be a source of metarsalgia and is characterized by pain in the forefoot. Sesamoiditis is located on the plantar surface of the foot and will be located near the first metatarsal phalangeal joint.
The ezWalker® Custom Performance Insole can help relieve the pain and pressure of hammer toe by strategically supporting the medial, lateral, and trans-metatarsal arches to relieve pressure on the ball of the foot and therefore, release the action causing the hammer toe in the first place. Each ezWalker Performance Insole is custom molded to the specifications of each one of your feet, providing you with the support and comfort you need to relieve pain and produce comfort. Whether your hammer toe condition is due to genetics or not, ezWalker® Custom Performance Insoles can help you find relief from hammer toe and foot pain. The back of your ankle may feel tight and sore.
These conditions include different types of arthritis , osteonecrosis , neuromas , tumors, or infections. Lastly, traumatic injuries, including fractures and ligament tears, can cause this type of foot pain. Treatment of foot pain often consists of anti-inflammatory medications , footwear modifications, and inserts for your shoes. When buying footwear, look for shoes with a wide toebox, good support, and avoid high heels. These pads help to take pressure off the ball of the foot. If some simple steps do not alleviate your symptoms, you should see your doctor to ensure you are receiving adequate treatment. In some rare situations, patients don't find relief with shoe modifications, and may require a surgical procedure. Remember that our shoes protect us from injury.
When the tissue of the arch of the foot becomes irritated and inflamed, even simple movements can be quite painful. Plantar fasciitis is the name that describes inflammation of the fibrous band of tissue that connects the heel to the toes. Symptoms of plantar fasciitis include pain early in the morning and pain with long walks or prolonged standing. Arch pain early in the morning is due to the plantar fascia becoming contracted and tight as you sleep through the night. Bunions develop from a weakness in the bone structure of your foot.

Rheumatoid arthritis causes forefoot deformity and often may cause displacement and even dislocation of the metatarsal joints themselves. Morton's Neuroma can also be a source of metarsalgia and is characterized by pain in the forefoot. Sesamoiditis is located on the plantar surface of the foot and will be located near the first metatarsal phalangeal joint.

The ezWalker® Custom Performance Insole can help relieve the pain and pressure of hammer toe by strategically supporting the medial, lateral, and trans-metatarsal arches to relieve pressure on the ball of the foot and therefore, release the action causing the hammer toe in the first place. Each ezWalker Performance Insole is custom molded to the specifications of each one of your feet, providing you with the support and comfort you need to relieve pain and produce comfort. Whether your hammer toe condition is due to genetics or not, ezWalker® Custom Performance Insoles can help you find relief from hammer toe and foot pain. The back of your ankle may feel tight and sore.